Bone grafting for dental implant is a common procedure that rebuilds lost jawbone so implants can be placed safely and last longer. This post explains what the procedure is, why and when it’s needed, the types of grafts, the typical healing timeline, what to expect during recovery, costs and risks, and how to choose the right provider.
What is bone grafting for dental implant?
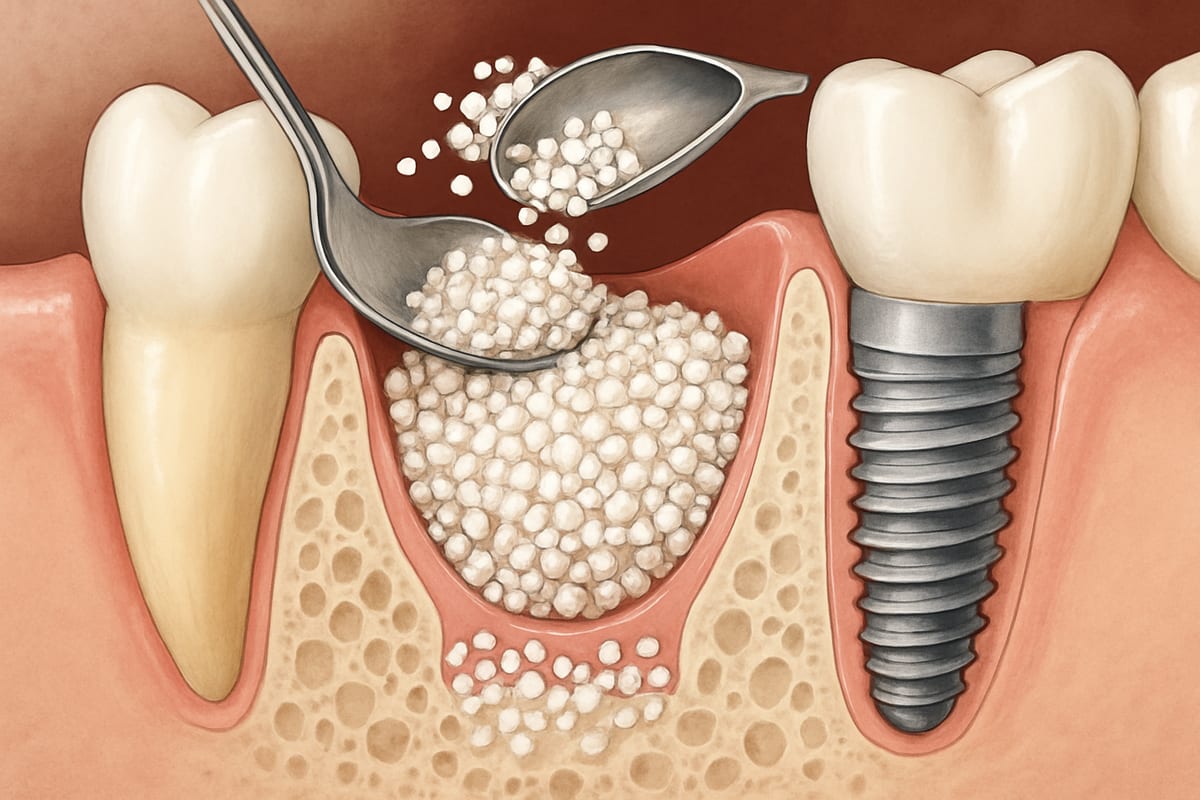
Bone grafting adds bone or bone-like material to areas of the jaw that have lost volume. The added material becomes a stable foundation for a dental implant, helping the implant fuse with the jaw and support a replacement tooth or full-arch restoration. Grafting can be done before implant placement or at the same time, depending on how much bone is available and the treatment plan.
Why you might need bone grafting
Common causes of jawbone loss
- Tooth loss: when a tooth is missing for a long time, the bone that held it shrinks.
- Infection: untreated tooth or gum infections can destroy bone.
- Trauma: accidents that damage teeth or the jaw.
- Long-term denture wear: ill-fitting dentures can accelerate bone loss.
Signs you may need a graft
Some signs that bone grafting may be necessary include loose or ill-fitting dentures, a sunken facial appearance near missing teeth, or imaging (X-ray or CBCT) that shows insufficient bone volume for an implant. Your dentist will review images and measure bone thickness to decide if grafting is required.
Types of bone grafts and pros/cons
Autograft (your own bone)
An autograft uses bone taken from elsewhere in your body, often the chin or the back of the jaw. Pros: high success because it’s your own living bone. Cons: requires a second surgical site and more recovery time.
Allograft (donor human bone)
An allograft uses processed human donor bone. Pros: no second surgical site, readily available. Cons: slightly longer healing time than autograft, though success rates are high when placed correctly.
Xenograft (animal-derived) and synthetic options
Xenografts (usually bovine) and synthetic materials (like calcium phosphate) act as a scaffold for new bone to grow. Pros: low morbidity, abundant supply. Cons: they often take longer to integrate and may not provide the same short-term strength as autografts.
Typical healing timeline
Healing depends on graft type and location. Small grafts can integrate in about 3–4 months. Larger grafts or sinus lifts may need 6–9 months before an implant is placed. Some cases allow simultaneous graft and implant placement, shortening total treatment time.
Procedure, recovery, costs, risks, and finding care
What happens before and during the procedure
Before surgery you’ll have a consultation with imaging (X-rays or CBCT) and a treatment plan. Medical history and any medications are reviewed. During the procedure you’ll receive local anesthesia, sedation, or general anesthesia based on the plan. The dentist or surgeon exposes the bone, places the graft material (and sometimes a membrane), and closes the site with sutures. If an implant is placed at the same time, it will be positioned to fit the planned restoration.
Recovery and possible complications
- Normal: swelling, mild to moderate pain, bruising, and light bleeding for a few days.
- Care: follow-up visits, soft diet, and avoiding pressure on the graft site help healing.
- Watch for complications: increasing pain, persistent swelling, fever, or drainage may signal infection and need prompt care.
- Risk factors: smoking, uncontrolled diabetes, or poor oral hygiene lower success rates.
Costs, insurance, and alternatives
Cost varies by graft type, size, and provider. Small grafts cost less; large reconstructions or multiple sites cost more. Dental insurance may cover part of the procedure, but many plans limit coverage for grafting. Alternatives or adjuncts include ridge augmentation, shorter implants, or angled implants that make use of remaining bone. Your provider can review options and a cost estimate based on your specific needs.
How to choose a provider for bone grafting for dental implant
Look for a provider with specific training in implant surgery—an oral surgeon, periodontist, or a dentist with advanced implant education. Ask about:
- Experience with the specific graft type you need and success rates.
- Use of modern imaging like CBCT for accurate planning.
- What anesthesia or sedation they offer and post-op care plans.
- Before-and-after photos and patient references for similar cases.
Schedule a consultation to review your images, treatment timeline, materials, and a written cost estimate. A clear plan helps you weigh benefits and risks and sets realistic expectations for recovery and outcomes.
Bone grafting for dental implant is a well-established way to rebuild the jaw and enable predictable implant success. With the right diagnosis, materials, and experienced provider, most patients achieve a strong, lasting foundation for dental implants.