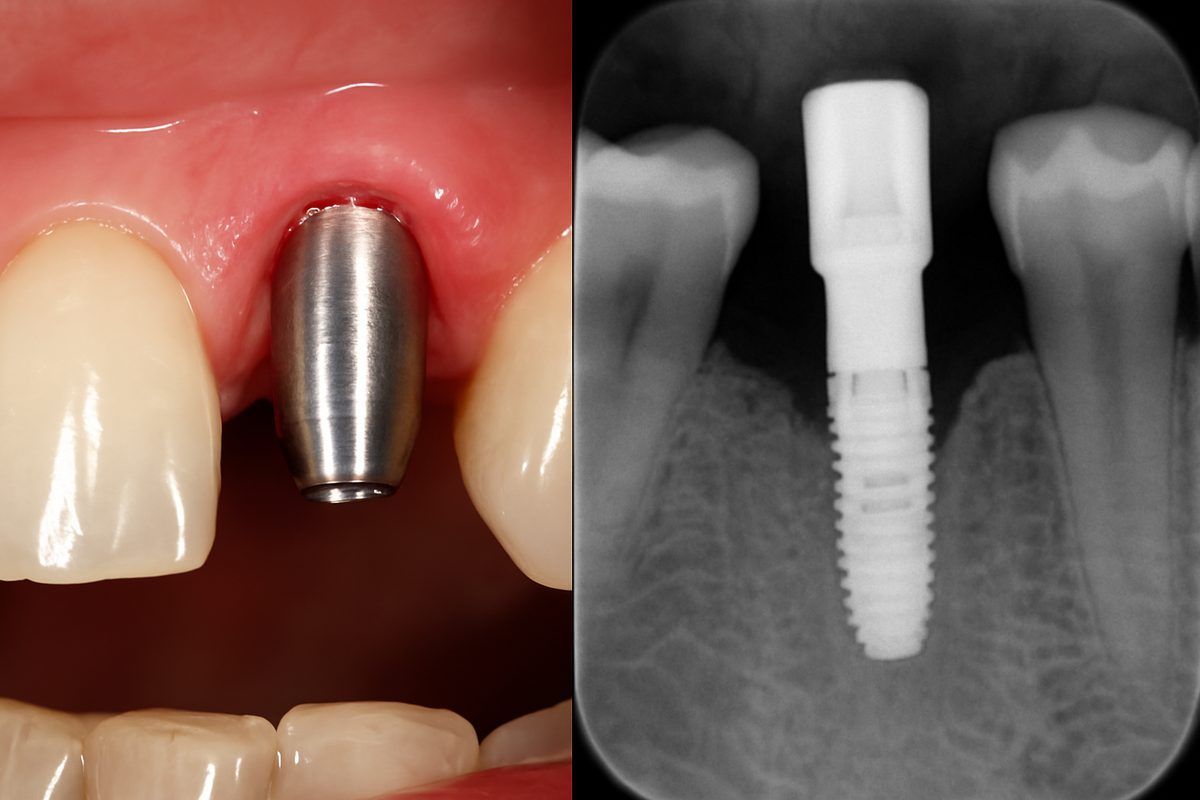
If you can see metal or feel a hard post under your gum, you may have a dental implant abutment exposed. This article explains what that means, why it matters for your health and comfort, and the steps you can take next. Read on to learn common causes, signs to watch for, how dentists diagnose an exposed abutment, treatment options, prevention tips, and when to seek urgent care.
Common causes of a dental implant abutment exposed
Gum recession
Tissue can slowly pull back over time, revealing the abutment. Recession may result from thin gums, aggressive brushing, or natural aging.
Poor healing or failed osseointegration
If the implant doesn’t fully fuse with the jawbone, surrounding tissue can shrink and expose the abutment. This weak integration may cause pain and instability.
Trauma or injury
A fall, sports hit, or heavy bite force can tear or bruise soft tissue and make the post visible.
Ill-fitting restoration or excess pressure
A crown or bridge that doesn’t fit well can place too much load on the implant and damage gum tissue, leading to exposure.
Poor oral hygiene and infection
Plaque buildup and peri-implantitis (gum infection around implants) cause inflammation and tissue loss that can reveal the abutment.
Signs and symptoms to watch for
Visible metal or abutment showing
You may see the post or a dark line at the gum level.
Pain, swelling, or bleeding
Irritation, soreness, and gum bleeding are common with exposure.
Loose crown or implant mobility
A loose restoration or a feeling that the implant moves are red flags.
Bad taste, pus, or signs of infection
Discharge, persistent bad taste, or fever require prompt attention.
How dentists diagnose an exposed abutment
A clinical exam with intraoral photos checks what’s visible. X-rays or cone beam 3D imaging show bone level and implant position. Dentists also test the fit of the prosthesis and evaluate bite forces and gum health.
Treatment options for a dental implant abutment exposed
Non-surgical care
Mild cases may improve with deep cleaning, better home care, and a short antibiotic course to control infection.
Soft-tissue grafting
Gum grafts can cover the exposed abutment, restore contours, and protect the implant long-term.
Adjusting or remaking the crown/abutment
Fixing a poor fit or correcting the bite reduces pressure on the tissue and prevents further damage.
Implant revision or removal
If the implant is infected or failed, removal and later replacement may be needed. This is more involved but sometimes necessary.
Emergency care
Severe pain, spreading infection, or swelling that affects breathing or swallowing needs urgent dental or medical care.
Prevention: how to avoid an abutment becoming exposed
Keep excellent daily oral hygiene and attend regular dental check-ups. Stop smoking and control health risks like diabetes. Use a nightguard for grinding and wear protective gear for sports. Seek prompt care for any trauma or looseness.
When to seek care
Seek same-day care for severe pain, swelling, pus, or sudden mobility. For non-urgent concerns, schedule an evaluation within a few days. Routine implant check-ups every 6–12 months help catch problems early.
About advanced care options and choosing the right provider
For complex implant problems, specialists using CBCT (3D) imaging, intraoral cameras, digital scanning, and guided planning get better outcomes. Soft-tissue grafting and precision restoration reduce recurrence. Signature Smiles Dental Group and Dr. David Shirinian offer concierge-style implant care with CBCT, iTero scanning, lasers, and in-house 3D tools to diagnose and treat exposed abutments.
Next steps / short CTA
If you suspect a dental implant abutment exposed, book an evaluation soon. Bring recent x-rays or implant records if you have them. Timely diagnosis and treatment greatly improve the chance of saving the implant and restoring healthy tissue.